Measuring Innate Immune/Phagocytic Cell Function by Flow Cytometry
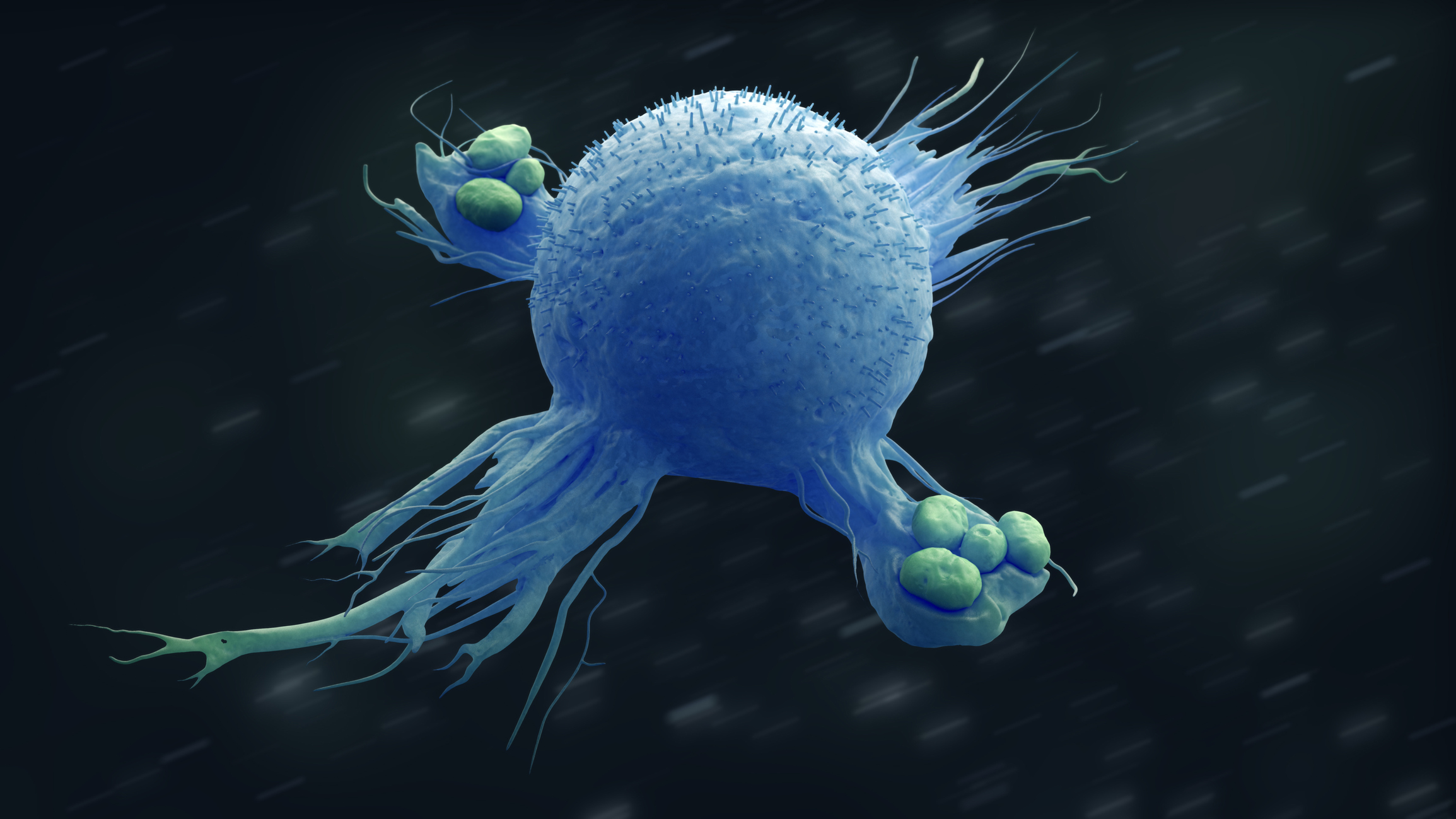
Our immune system is in a constant “molecular arms race” to stave off pathogenic invaders that want take up residence in our bodies. This is a battle where the microbes may gain the upper hand for a time, only to be outmaneuvered by our immune cells (Jonas, 2019). For an immune cell, one strategy and ancient mechanism in this fight is to simply engulf and eat the invaders. Phagocytosis (from Ancient Greek φαγεῖν (phagein), meaning ‘to devour’, κύτος, (kytos), meaning ‘cell’, and -osis, meaning ‘process’) is the process for the ingestion and elimination of pathogens and apoptotic cells by specialized cells of the innate immune system called phagocytes. Not only are phagocytes the first line of defense against invading microbial pathogens, they also play an important role in tissue homeostasis by removing apoptotic bodies, senescent cells and cell fragments (Gray, 2017). Professional phagocytes include monocytes, macrophages, neutrophils, dendritic cells, osteoclasts, and eosinophils (Rosales, 2017).
The phagocyte recognizes pathogens (or debris) for engulfment and clearance by specialized receptors on its cell surface. The process of Phagocytosis begins with the binding of opsonins (i.e. complement or antibody) and/or specific molecules on the cell surface of the pathogen (called pathogen-associated molecular patterns or PAMPs) to cell surface receptors on the phagocyte (Figure 1).

Figure 1. The phases of the phagocytic process. Phagocytosis is divided into four main steps: (i) recognition of the target, (ii) signaling to activate the internalization machinery, (iii) phagosome formation, and (iv) phagolysosome maturation. The phagolysosome is a specialized acidic and hydrolytic environment that degrades the engulfed particle.
The best characterized opsinic receptors on phagocytes are Fc Receptors (FcR) and complement Receptors (CR). Non-opsinic receptors on phagocytes include pattern recognition receptors (PPR), such as Toll-Like Receptors (TLR). The phagocyte also has receptors (TIM-1, TIM-3) for the recognition of phosphotidylserine on apoptotic cells that marks them for clearance (Rosales, 2017).
Reactive oxygen species (ROS) are generated during Phagocytosis and in response to soluble agonists such as fMLP (N-formyl-met-leu-phe, a potent activator of innate immune cells). This response is called the Respiratory Burst and is crucial to the destruction of pathogens by phagocytes. The phagocyte converts molecular oxygen to superoxide anions (via NADPH Oxidase), which are then converted to ROS. ROS have very potent anti-microbial activity. Without the ability to generate ROS, subjects face lifelong susceptibility to infection. There are some neutrophil shortage and functional disorders that arise from genetic mutations that demonstrate this profound immunodeficiency. Chronic Granulomatous Disease (CGD) results from a genetic defect in NADPH Oxidase function (Epling, 1992). Patients with CGD have impaired Respiratory Burst function which predisposes them to bacterial and fungal infections. Certain drugs may also modify innate immune functions and put subjects at risk for infection. For example, a decrease in white blood count is a side effect of many chemotherapies, and because of their rapid turnover, neutrophils are especially susceptible to this effect. The resulting Neutropenia puts patients at risk for serious and even life-threatening infections, and their immune status must be constantly monitored.
The assessment of Phagocytosis and the Respiratory Burst Response is an important Indicator of overall innate immune cell health and can be done with streamlined flow-cytometry based assays.
FCSL is currently developing two flow-cytometry based assays to assess innate immune function. The first assay is the Monocyte/Neutrophil Respiratory Burst assay. Briefly, blood samples are exposed to Phorbol 12-Myristate 13 Acetate (PMA), a potent agonist to induce ROS and Red Blood cells (RBC) are lysed prior to acquisition of cells on the flow cytometer. ROS are evaluated in gated neutrophils and monocytes by measuring the fluorescent signal of dihydrorhodamine 123, a dye indicating the presence of ROS within these cells. Lymphocytes are used as control cells as they do not produce ROS like monocytes and neutrophils
The second flow-cytometry based innate immune cell assay measures Phagocytosis by both monocytes and neutrophils. DyLight 405™-labeled Rabbit IgG-opsonized latex beads are incubated with whole blood samples for 1-4 hours. A surface antibody (CD14) and light scatter are used to identify monocytes and neutrophils on the flow cytometer. Phagocytosis is measured by the uptake of Latex beads (DyLight 405™ fluorescent signal) within these populations.
We will be presenting poster #534 at the upcoming ISAC CYTO2019 Meeting June 22 – 26 in Vancouver, BC. This poster will illustrate how phagocytosis and respiratory burst assays can be used to evaluate innate immune cell function from non-clinical and clinical studies or be used for drug screening purposes, in vitro. Contact us to start a scientific discussion on how these assays may be useful for your drug development programs.
References:
Dinauer, MC, 2016, Primary Immune Deficiencies with Defects in Neutrophil Function, Hematology, 43-50.
Rosales C., Uribe-Querol E. 2017, Phagocytosis: A Fundamental Process in Immunity, BioMed Research International, 1-18.
Gray, M., Bothelho RJ, 2017, Hungry, Hungry Cells, Methods Mol Biol, 1519: 1-16.
Pauwels AM, Trost M, Beyaert R, Hoffmann E. 2017, Patterns, Receptors, and Signals: Regulation of Phagosome Maturation. Trends Immunol. 38(6):407-422.
Chen, Y., Junger WC, 2012, Measurement of Oxidative Burst in Neutrophils, Methods, Mol Bio, 844: 115-124.
Jonas A., Bonsignore P., Hammer, S., Frickey, T., Hauck, C. 2019, Adaptation to Host-Specific Bacterial Pathogens Drives Rapid Evolution of a Human Innate Immune Receptor. Current Biology.

