Exhausted T cells
T cell exhaustion is a state of dysfunction that arises during chronic infection and cancer. When exposed to persistent antigen and/or inflammatory conditions, T cell function falters and declines to the eventual state of exhaustion. T cell exhaustion was first described for CD8+ T cells and most studies have focused specifically on CD8+ T cells, but CD4+ T cells can also develop an exhausted phenotype (Saeidi, 2018). Exhaustion is defined by poor effector function, the sustained expression of multiple inhibitory receptors (IR), reduced proliferative capacity, and an altered transcriptome that is distinct from that of functional effector or memory T cells (Wherry and Kurachi, 2015, Wherry, 2011). T cell exhaustion was first observed in mice infected with lymphocytic choriomeningitis virus (LCMV), where persistent virus shut down or eliminated virus specific cytotoxic CD8+ T cells. T cell exhaustion has also been described clinically in Human Immunodeficiency Virus (HIV), Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), and cancer. Because antigen-specific CD8+ T cells control chronic infections and cancer, exhaustion leads to a pathogen/host stalemate and inefficient control of infection and tumors.
Checks and Balances
The immune system must be able to distinguish between danger and non-danger signals and carefully balance activation with deactivation. On one hand, it must mount an appropriate response against pathogens or cancer, but on the other hand, the immune system must be able to deactivate because sustained or exaggerated T cell responses can result in autoimmunity, allergy and cancer (Figure 1.)

Figure 1. Exaggeration of T cell responses can result in immunopathologies including Autoimmunity, Allergy, and Cancer. Graphic courtesy of Jiseong Kim.
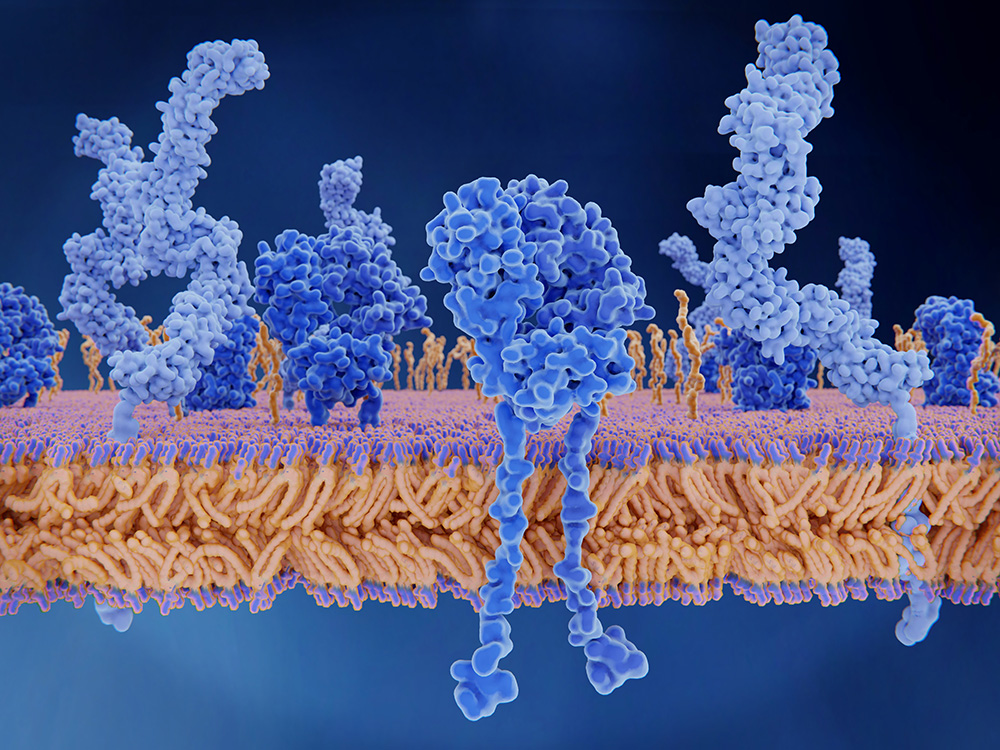
One mechanism to prevent overstimulation is for effector cells to upregulate inhibitory receptors (IR) on their cell surface such as PD-1, CTLA-4, LAG3, TIM3, TIGIT, CD244, CD160 and others. While IR provide an important check on the immune system, this same mechanism can be exploited by virus and cancers to avoid the immune system. For example, in human diseases with persistent high antigen exposure such as HIV, HCV, and cancer, the inhibitory molecules, PD-1 and CTLA-4 are over expressed on T cells. The sustained expression of multiple inhibitory receptors is the hallmark of exhausted T cells (Figure 2).

Figure 2. Inhibitory and co-stimulatory molecules and their receptors. Immune checkpoints are proteins that act as T cell receptor (TCR) co-signaling partners that deliver either positive or negative signals to T lymphocytes. Inhibitory molecules are shown from the top and marked with red blockades on the T cell, while co-stimulatory molecules are shown below and marked with green arrows. Under normal conditions, these proteins are critical for self-tolerance, but in tumors these immune checkpoint proteins can allow the tumor to evade the antitumor immune response. Blocking the actions of these proteins can produce a potent antitumor response. Graphic courtesy of Jiseong Kim.
Normal and Impaired Effector/Memory Differentiation and Exhaustion
After an initial infection, naïve T cells are activated and over the next 1-2 weeks, differentiate into effector cells. Proliferative and transcriptional changes result in their evolution into T cells with effector function and tissue homing abilities. After peak effector function, antigen clearance and the resolution of inflammation, most cells die. But, 5-10% of the cells persist as the memory T cell pool. Memory cells (aka antigen experienced T cells), down regulate their effector function, but can reactivate and proliferate upon reencounter with antigen.
Under normal conditions, memory T cells develop antigen independent self-renewal (driven by IL-7 and IL-15). Exhausted T cells have low expression of CD122 (beta chain of IL-2 and IL-15 receptor), and CD127 (IL-7 receptor alpha chain), thus they can’t respond to these cytokines. There is diversity in this memory pool: Memory T cells can be either effector (TEM) or central memory cells (TCM). TCM express CD45RO, CCR7 and CD62L and are found in lymph nodes and the periphery. TEM express CD45RO, but don’t express CCR7 and CD62L: thus they lack lymph node homing receptors and are found in the periphery and tissues.
In contrast, in conditions of persistent antigen exposure, memory programming is altered during the progression from effector T cell to memory cell. This altered differentiation results in T cell exhaustion. This is demonstrated in the in the mouse LCMV model. When CD8+ T cells are primed during infection with chronic LCMV, and then removed after 1 week of exposure to the infection, they can still differentiate into fully functional CD8+ memory T cells. But, when they are exposed to persistent antigen for 2-4 weeks, they become exhausted, and cannot recover normal memory differentiation once removed from antigen exposure (Wherry and Karachi, 2015). The severity, duration of antigen, and the loss of help from CD4+ T cells, lead to more severe exhaustion. For example, in HIV, CD8+ T cell exhaustion worsens in the absence of CD4+ cells and IL-21. Infections also lead to disruption of the lymphoid architecture and are associated with pathogenesis and poor immunity, as it impairs trafficking and interactions with cells necessary for T cell function.
Using Flow Cytometry to Phenotype Exhausted T Cells
How do we identify exhausted T cells? This is where the power of flow cytometry comes in. Flow cytometry can be used to phenotype both the surface markers and intracellular markers of exhausted T cells. As described earlier, common to both CD4+ and CD8+ exhausted T cells is the surface expression of multiple IR: PD-1, CTLA-4, LAG-3, TIM3, CD244, CD160 and TIGIT, and others (Figure 3). Exhausted T cells have decreased intracellular TNFα and INFγ. Exhausted CD4+ T cells become skewed towards a Tfh (T follicular helper cell) phenotype and express the surface markers CXCR5 and ICOS. Normal CD8+ effector T cells co-express the transcription factors T-bet (T-box transcription factor), and EOMES (eomesodermin), while exhausted T cells express one or the other of these factors. Two exhausted CD8+ T cell populations have been defined: the first is EOMEShigh PD-1high, TIM3+ and CD160+, has high granzyme expression, but limited proliferation capability (Wherry and Karatchi call these cells the “the severely exhausted”). The second population is T-bethigh PD-1low, has low proliferative capacity, and can still secrete TNFα and INFγ (Catkovic, 2017, Wherry and Karatchi 2015). And, the plot thickens: unexpectedly, it is recently reported that a subset of exhausted CD8+ T cells express SIPRα, a protein whose expression was previously thought to be limited to myeloid cells (Myers, 2019).

Figure 3. Graphical representation of an exhausted T cell with the common surface inhibitory markers present in this state illustrated. Graphic courtesy of Jiseong Kim.
Reviving Exhausted T cells
Reviving exhausted T cells holds much therapeutic promise. Targeting PD-1 and other over expressed inhibitory markers is a good strategy to reverse exhaustion. “Blockade of the PD-1 pathway has opened a new therapeutic avenue for reinvigorating T cell responses, with positive outcomes especially for patients with cancer” (Hashimoto, 2018). It has been shown that a combined blockade of PD1–B7-H1 (PDL-1), with other co-inhibitors, most notably TIM3, CTLA-4 and LAG3, has a synergistic effect in reversing exhaustion (Chen and Flies, 2013). The combination of IL-2 with PD-1 inhibition during chronic infection invigorated exhausted T cells. Also, an agonistic monoclonal antibody specific for 4-1BB (CD137) in combination with IL-7 restored the activity of dysfunctional CD8+ T cells in the LCMV mouse model (Wherry and Karachi, 2015).
However, there is a flipside: it’s been shown that when T cell exhaustion is reversed, mice develop autoimmune disease and die from CD8+ T-cell mediated immunopathologies such as lymphoproliferative disorders and multi-tissue destruction. Also, CTLA-4 blockade in murine models of diabetes and multiple sclerosis (MS) results in an increased inflammatory response (Catkovic, 2017).
And, finally, in some situations exhausted T cells can be beneficial: in patients with autoimmune diseases, exhausted T cells correlate with favorable prognosis (Catkovic, 2017). And in transplant, persistence of exhausted recipient CD8+ T cells correlated with better therapeutic effect (David, 2019).
At FCSL, we recognize the exciting biology and ongoing research involving T cells and their inhibitory receptors, and are privileged to play a part in the development of new immunotherapies designed to benefit patients with chronic diseases. We are a contract flow cytometry lab and routinely run up to 10-color flow cytometry panels supporting basic research, non-clinical and clinical studies. We are experts in flow cytometry panel design, including fit-for-purpose flow cytometry panels, Immunophenotyping, Receptor Occupancy Assays (ROA), and the inclusion of proprietary markers into established flow cytometry panels. If your research involves T cells, or targeting immune checkpoints, please contact us for more information.
References:
Catkovic K., 2017, T cell exhaustion: from Pathophysiological Basics to Tumor Immunotherapy,
Cell Communication and Signaling, 15:1-16.
Chen L., and Flies, DB, 2013, Molecular Mechanisms of T cell co-stimulation and Co-Inhibition, Nat Rev Immunol 13: 227-242.
David, P. 2019, The PD-1/PDL-1 Pathway Affects the Expansion and Function of Cytotoxic CD8+ T cells During Acute Retroviral Infection. Frontiers in Immunology, 10: 1-13.
Hashimoto, M., 2018, CD8 T cell Exhaustion in Chronic Infection and Cancer; Opportunities for Interventions. Ann Review of Medicine 69: 301-318.
Meyers, LM, 2019 A Functional subsets of CD8+ T cells during chronic exhaustion is defined by SIPRα. Nat Comm, 10,794: 1-15.
Pennock, ND, 2013, T cell responses: Naïve to memory and everything in between, Adv Physiol Educ 27 (4) 273-282.
Saiedi, A., 2018, T-Cell Exhaustion in Chronic Infections: Reversing the State of Exhaustion and Reinvigorating Optimal Protective Immune Responses, Frontiers in Immunology, 9: 1-12.
Wherry EJ and Kurachi M., 2015, Molecular Insights into T cell Exhaustion, Nature Review Immunol, 15: 486-499.
Wherry, EJ, 2011, T cell Exhaustion, Nature Immunology, 12: 492–499.
Wykes M. and Lewin, SR, 2018, Immune checkpoint blockade in Infectious Diseases, Nature Reviews Immunology, 18: 91–104.

