Creating Consistent Results by Managing your Flow Cytometry Data
If you are looking to incorporate flow cytometry into your study or clinical trial, ensuring that precise and uniform data is generated by contract flow labs can seem difficult, or even overwhelming. In fact, a study conducted by Maecker et al. 2005 revealed that in a protocol conducted across 15 different laboratories, the inter-laboratory coefficient of variation in results was between 17 and 44%. With such a high possibility for variability in even straight forward immunophenotyping data, the prospect of generating accurate results through contract flow labs may seem daunting. However, managing the flow cytometry services in your study is possible, and by partnering with an experienced flow cytometry team, even more achievable.
Choosing the correct contract flow lab can be difficult in and of itself, depending on what is important in a particular study, or to the research organization. While both large and small contract research organizations (CROs) have benefits, each must be assessed to determine the best fit. The table below summarizes a few pros and cons.

While large CROs offer many services and market themselves as “one stop shops”, they may not be the top experts in these services. Broad service offerings can indicate shortcomings in depth of expertise. For example, you might be wary if an ear, nose, and throat doctor started offering elbow treatment in an effort to expand.

Larger CROs have a global footprint to conduct huge studies, but their processes become more rigid over time. Policy, senior management involvement, established work processes, internal resources, and more can often show up as roadblocks in the path of innovation. A large organization lacks flexibility, personal service and innovation, and very often the status of its size doesn’t improve the quality of the research or the value of a partnership. On the other hand, a specialized and small CRO has the innate capacity to focus study teams and management time on numerous and varied projects. They have a specialized team of scientists and individual staff that have top of the line expertise in one particular area and stay at the forefront of their respective fields. They also have an enhanced ability to make quick decisions and adapt to changes in a project on the fly.
Certainly, there are many components of the flow cytometry process that can lead to differing data results among labs, or even among analysts in the same lab. Through the entire process, from specimen shipping, sample processing, and up through data analysis, slight variations can have an impact results.. This may occur despite the fact that the same samples and reagents were used in each case. Potential large variation in the study is indicative that flow cytometry assays are one of the most challenging of all analytical assays to transfer. Because of this, the testing facility must ensure that the assay meets pre-determined standards, performs reliably and is fit for its intended use. Since there is no one-size-fits-all approach given the variable conditions – multiple instruments, multiple platforms or multiple site environments – it is very important to standardize as many variables as possible. Luckily, the flow cytometry scientific community is coming together to create universal standards to which test sites can hold themselves..
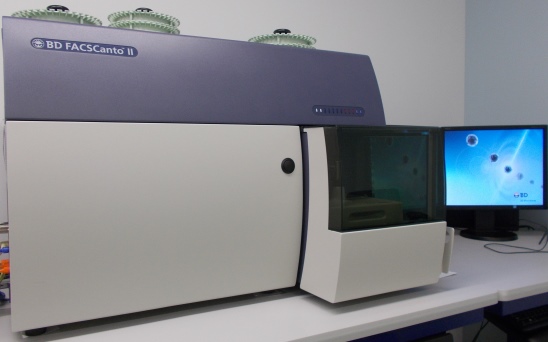
Instrument setup and quality control (QC) is imperative, especially when different types of instruments at different facilities are being used. This QC should be performed daily, and can be performed with calibrated beads with predetermined reference ranges. All cytometers should fall within these ranges so that uniformity of function can be validated. Make sure any lab you contract performs regular QC of instrumentation, and keeps the cytometers cleaned and up-to-date on maintenance.
As with the quality control of the instruments, strict guidelines must be adhered to for reagents as well. Critical reagents require certificates of analysis or material data sheets to verify storage conditions and usage records, in addition to verifying the source and quality of the specific reagent. Standardizing reagent clones, flourophores and panel implementation also goes a long way to ensure comparable results between laboratories.
Before a sample even arrives at a testing facility, its stability can be affected in ways that impact the final data. For example, the anticoagulant used in a shipped sample may change aspects of the specimen itself. In one case, heparin can affect the morphology of a sample by causing cells to clump together, but its other benefits may make this a preferred anticoagulant for some analyses. Just like heparin, EDTA is a common anticoagulant for transportation, but it can affect the sample by binding with divalent cations. More important than the anticoagulant itself is uniform use of the same compound for all samples in a study, so that any impacts are consistent among specimens. Storage and transportation temperature are also critical requirements for sample stability. Too high or low storage temperature will increase the degradation rate and render samples unfit for analysis. Most vital, a test site should validate samples after shipment and test their stability over time to understand how length of time post-draw impacts cell populations. As long as a test site understands how time affects results and decides upon a window in which it is acceptable to test a sample, variation in this area can be minimized.

Sample processing must be rigorously planned and uniform in order to ensure consistent results. Prior to any assay performance, procedures should be in place to maximize uniformity between the samples. When samples are from the early stages of drug development, method validation is not necessarily required. Method qualification, however, is an excellent tool to ensure the results of the data are consistent and reproducible, which is desired no matter the stage of drug development. Later-stage studies must be kept GLP and FDA compliant, and require method validation be performed prior to the study starting. For both method qualification and validation, the correct anticoagulant and tube type must be decided upon and stability must be monitored to designate whether a preservation tube must be chosen over a standard blood collection tube. Sample type must be taken into consideration as well, as both whole blood and peripheral blood mononuclear cells can be used in flow cytometry.

For more information on specimen stability, sign up to receive our free Stability Guide. The banner on the homepage has the sign up information.
FCSL is a contract flow lab that provides high throughput and high capacity flow cytometry services, running multiple flow cytometers with up to 10 color antibody panels daily. We are proficient in processing a multitude of specimen types including whole blood, frozen PBMCs along with cell culture and tissue processing capabilities. Our flexibility in handling so many specimen types allow for the support of a wide range of flow cytometry assays including: immunophenotyping/lymphocyte subset analysis, receptor occupancy, functional assays and cell viability/apoptosis measurements. Our expert staff is always available to help guide you through these tests and we welcome clients to visit our facility. We encourage sponsor engagement throughout the process. Contact us for more information!
References
Duggan, Ryan. “UCFlow – Flow Cytometry News, Reviews, and Tips.” The NovoCyte Analyzer Review – Acea Biosciences, 25 Sept. 2015, ucflow.blogspot.com/2015/09/the-novocyte-analyzer-review-acea.html.
Lee, Tyler et al. “EDTA for Battery Reconditioning.” Fact Battery Reconditioning Blog, 2015, factbatteryrecon.com/2015/06/03/edta-for-battery-reconditioning-10/.
Maecker, H. T. et al. Standardization of cytokine flow cytometry assays. BMC Immunol. 6, 13; doi: 10.1186/1471-2172-6-17 (2005).
Van Der Strate, Barry et al. “Best Practices in Performing Flow Cytometry in a Regulated Environment: Feedback from Experience within the European Bioanalysis Forum.” Bioanalysis, vol. 9, no. 16, 2 Aug. 2017, pp. 1253–1264., doi:10.4155/bio-2017-0093.

